Imagine going under surgery without anesthesia. Undoubtedly, fear among patients scheduled for surgical procedures is pervasive. Some professionals even attribute patient anxiety to the fear of the anesthetic itself but understanding how doctors administer anesthesia can be incredibly beneficial to easing the tension of a worried patient. After all—the more we know, the less we fear.
Anesthesia machines are one of the most versatile medical instruments in the healthcare industry. The pneumatic devices help doctors sedate their patients before surgery and keep them asleep, while breathing, throughout the procedure. Primarily, the function of the anesthesia machine is to help surgeons mitigate their patient’s pain during a medical operation. In this sense, anesthesia machines become a patient’s knight in shining armor, but few people understand the device’s inner workings.
What is an Anesthesia Machine?
An anesthesia machine is a pneumatic device that supplies a mixture of oxygen, gas, and anesthetic agent to a patient, allowing them to remain unconscious, but breathing, during surgery. The device delivers oxygen while simultaneously ensuring that the patient does not inhale the life-threatening CO2 they previously exhaled. Surprisingly, however, the anesthesia machine’s design has remained relatively the same since its invention. The essential components of an anesthesia machine include:
The Ventilator: used to keep the patient breathing during surgery.
Breathing Circuits: to keep the air and gasses flowing to and from the patient safely.
Scavenging Systems: to remove the “used” gasses such as CO2.
Safety Mechanisms: to ensure a patient’s well-being in the case of an emergency.
Here is an in-depth look into how each component works in an anesthesia machine.
The Ventilator
Ventilators are an important part of all anesthesia machines. The ventilator is essentially a set of external lungs. It breathes for deeply anesthetized patients, maintaining the patient’s regular respiratory rates and blood chemistry. In the beginning automatic ventilators were very simple with few modes of ventilation. As time passed, ventilators became more sophisticated with many advanced ventilation modes, having either a double circuit, bellow design, turbine design or a single circuit piston configuration.
The latest technology coming into the market is the volume exchanger, an innovative breathing system that delivers precise and reliable ventilation to patients with rapid wash-in and wash-out time. It offers less risk of malfunction with no moving components, providing increased reliability and a longer service life.
Breathing Circuits
The breathing circuits are the parts of an anesthesia machine that deliver the essential gasses to a patient and subsequently eliminate the CO2 exhaled. There are two kinds of breathing circuits: the non-rebreathing circuit and the circle circuit. Non-rebreathing circuits are exactly like they sound – the gasses, once exhaled, are eliminated from the system, and the patient does not rebreathe them. Circle circuits are the opposite – they remove the CO2 exhaled by the patient and allow the rebreathing of the exhaled anesthetic gasses.
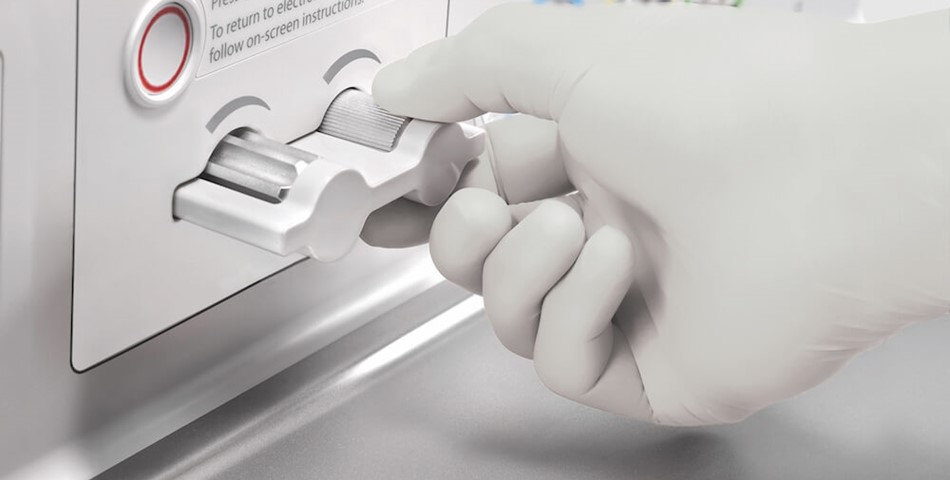
Within a breathing system, vaporizers help to add precise amounts of anesthetics to the gas flow. In most machines, the total gas flow enters the vaporizer, which splits the fresh gas into a carrier gas and a bypass gas. The carrier gas receives the anesthetic agent and then meets back up with the bypass gas before entering into the patient’s breathing circuit. Operators can control the ratio of the split to decrease or increase the gas concentration, thus controlling the amount of anesthetic a patient will receive.
Scavenging Systems
Scavenging systems in an anesthesia machine collect and expel anesthetic gases from the operating room. In an active system, suction removes gases. Passive systems allow the gas to escape through a ventilation exhaust. When anesthesia machines implore an active system, doctors must protect the patient’s airway from the suction device. By contrast, passive systems require only pressure monitoring. Anesthesia machines release a surprising amount of greenhouse gasses into the Earth’s atmosphere, hence the healthcare industry’s push towards low-flow delivery whenever possible.
Safety
An anesthesia machine has many alarms that inform the medical team when a patient might be entering a critical or dangerous state.
When a patient is connected to a ventilator during surgery, these “disconnect alarms” are activated. Anesthesia workstations boast at least three disconnect alarms: one that informs the team of low pressure in the breathing circuit, a second that notifies of a low exhaled tidal volume, and a third that cautions of low exhaled carbon dioxide. Each of these states could mean that the patient is in danger. Thus, doctors must closely monitor them to ensure the safety of the patient during surgery.
The latest machines also employ more electronically run components than ever before – meaning that it is essential to ensure that an anesthesia machine has at least a thirty-minute battery charge in the case of an unexpected power outage. Thirty minutes is plenty of time for a surgeon to close and an operator to “revive” a patient safely if there is a power emergency.
Anesthesia Monitoring Devices Market to Exceed US$ 3.4 Billion by 2027 Amid Rising Prevalence of Degenerative and Chronic Illnesses
The global anesthesia monitoring devices market is projected to grow from US$ 2.2 Billion in 2022 to US$ 3.4 Billion in 2027. As per the study, overall sales are slated to expand at an impressive CAGR of 9.1% over the forecast period (2022-2027).
Increasing number of surgical cases is likely to drive growth in the anesthesia monitoring devices market during the forecast period. Rising technological advancements and developments in the field of anesthetic delivery technology are also expected to drive growth in the anesthesia monitoring devices market. Moreover, surging desire for patients to undergo pain-free surgical operations is anticipated to support the expansion of the anesthesia monitoring devices market.
Rising prevalence of degenerative diseases and chronic illnesses has resulted in an increased dependence on surgeries and treatments. As a result of the rising need for continuous monitoring, the anesthesia monitoring devices market is set to expand.
Integrated devices developed by key players come with decision support and advanced monitoring capabilities that not only measure complicated parameters, including inhalation anesthetics, end-tidal carbon dioxide, oxygen concentrations, and transcutaneous oxygen saturation, but also provide data analysis to help doctors make surgical and therapeutic intervention decisions.