Ensuring healthcare accessibility is crucial because it establishes an environment that is approachable for individuals of diverse abilities, including those with vision impairments. Patients with visual impairment frequently encounter difficulty physically maneuvering in and around environments that are not designed to accommodate their unique needs. From the moment a patient enters the doors of your practice, they should feel comfortable and able to access the physical space and documented resources they need until the moment they leave to ensure a productive visit.
Maintaining the accessibility of optometry offices also guarantees that individuals of all visual capacities may receive essential eye care treatments. Optometry offices that prioritize accessibility allow patients with ocular diseases to receive necessary care for diseases such as glaucoma, diabetic retinopathy, and macular degeneration. Additionally, regular eye examinations are essential for effectively managing visual problems in individuals with low vision. Eye care providers have the expertise to prescribe corrective devices and low-vision aids and provide advice on lifestyle modifications that might improve the quality of life for people facing visual difficulties.
To enhance accessibility for patients with low vision in optometry offices, it is necessary to address the existing barriers. This article will explore a few methods to do so.
Physical environment improvements
Figure 1. An example of how high-contrast colors on a sign can make a difference in legibility. The yellow-and-black sign is easier to read than the green-and-blue sign. (Image courtesy of Euin Cheong, OD)
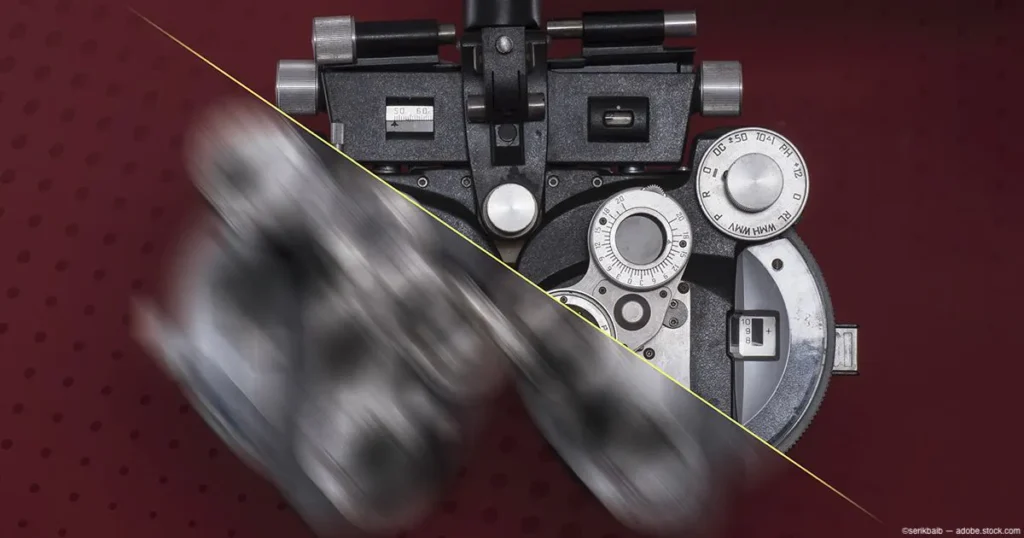
First, it is important to name methods that help establish a physically secure environment. Improving office signage can be a part of this process of achieving improved visual accessibility. Legibility of signage can be enhanced by using prominent, bold fonts on signs and printed materials. It is advisable to further consider the use of tactile signage. Ensure that signage is positioned at a height that is easily visible to individuals and in critical areas throughout the office to effectively direct patients. Opting for high-contrast colors, such as black text on a white or yellow background, facilitates readability compared with low-contrast colors, such as blue text on a green background
Reducing physical obstacles is another method of establishing a physically secure environment. This can be achieved by ensuring that the corridors and entryways are free from obstructions that may cause patients to collide with objects or one another, having smooth flooring to minimize tripping, and using furniture with distinct color contrasts to clearly define different regions of the office. Having well-illuminated areas with uniform illumination is crucial for minimizing both glare and shadows. Individual preferences can be accommodated by using adjustable lighting solutions.
Making paperwork accessible
When patients come in for eye examinations, there is typically at least some paperwork that needs to be signed. Forms such as these are typically written in a font style that is very small, with little space between each line. It can be quite challenging for most patients who have vision impairment to properly read the text presented on these forms. By making forms and educational materials available in large print, an office can make its services more accessible to people with vision impairment.3 It would also be useful to provide digital access through the office website or email, as many patients are able to make use of technological features such as zooming in or using text-to-speech options.
During the eye examination
When evaluating visual acuity in individuals with low vision, it is crucial to exhibit patience and tailor the examination to suit the specific needs of each person. It is important to select a testing methodology that is appropriate for the patient’s visual status.
Visual acuity
One of the primary challenges encountered during an eye examination is the process of measuring visual acuity. Commonly used visual acuity charts often only go to a level of 20/400 and/or jump to 20/800 or require the use of central vision only. Although it is common for technicians to rely on counting fingers to assess visual acuity, there are more accurate methods for obtaining precise visual acuity measurements. It is advisable to use charts that are specifically tailored for individuals with limited vision. These charts incorporate larger optotypes, increased spacing between optotypes, and enhanced contrast. Two examples of charts specifically created for patients with low vision are the Lighthouse and Feinbloom charts. Early Treatment Diabetic Retinopathy Study charts are versatile in that they allow for adjustments in distance similar to the previously mentioned examples. These charts allow accurate assessments of visual acuity regardless of how limited the patient’s vision may be.4
The same applies to near vision acuity testing. The conventional Rosenbaum pocket acuity card fails to adequately accommodate people with visual impairments. One way to improve the measurement of near visual acuity is by investing in more accessible charts, such as the MNREAD chart.
Medical examination
Additionally, we can implement strategies to accommodate patients with visual impairments, thereby ensuring a comfortable examination experience for them. First, it would be considerate to verbally guide patients through the various phases of the examination, as they might struggle to see our actions in their peripheral and/or central vision. Phrases such as “I will approach you closely with this bright light to examine your pupils” or “I am moving this instrument toward you; may I assist you in positioning your chin and forehead correctly?” allow the patient to maintain awareness of the situation and avoid feeling helpless in the examination room. Upon concluding the visit, it is crucial for the physician to deliver a verbal summary of the assessment and plan, as the patient might lack the means to access and read the online portals when reviewing their results or details of the visit.
Keep staff up to date on accessibility
When overseeing an optometric clinic, there are numerous subjects and competencies that necessitate staff training. Every eye care facility will inevitably encounter patients with low vision. Everyone on the staff, including receptionists, technicians, and medical assistants, should undergo training to be cognizant of the requirements of individuals with low vision to provide essential support. This is crucial for cultivating an inclusive and empathetic atmosphere. Technicians should be aware of the importance of reducing unnecessary transportation between testing and assessment rooms with such patients to minimize fatigue or risk of falling. As discussed above, it is also crucial to identify the appropriate use of specific visual acuity charts and verbally explain each step of the examination, including scans. Proper staff training will allow everyone to demonstrate respect and consideration while addressing patients’ needs.
Conclusion
To go above and beyond, consider the use of assistive devices and technologies to enhance the patient’s visual experience and address specific challenges associated with visual impairments. If this is not a possibility at the practice currently, collaboration with specialists in low vision can also provide valuable insights for optimizing visual function for individuals with low vision.
Access to eye care services can have a substantial impact on an individual’s ability to maintain their independence as well as their general quality of life. People with low vision can lead lives that are more meaningful if they can address concerns regarding their vision, obtain suitable visual aids, and receive recommendations on better engagement in daily activities. Ensuring that optometry offices are accessible to those with low vision is crucial for fostering equal access to health care, improving the management of eye diseases, allowing early detection of these diseases, and pursuing education and support that would yield improvement in the quality of life for individuals with visual impairments.